 Click to Print Adobe PDF
Click to Print Adobe PDF
Winter 2012 - Vol.7, No.4
|
Medicine on Ice: Therapeutic Hypothermia for Cardiac Arrest
Tom P. Shuman, B.S.
Research Intern, Radiation Oncology
Roy S. Small, MD, FACC, FSCAI
The Heart Group of Lancaster General Health
|
  |
INTRODUCTION
In August 2012, hundreds of Boy Scouts and parents gathered to celebrate the 40-year career of JW, a Scoutmaster in Lancaster County. For one of this article’s authors (TS), one of the more than 200 Eagle Scouts he had mentored during his lifetime of achievement in Boy Scouts of America, this milestone was even more impressive considering that he had “died” a few years earlier.
As one of the many victims of out-of hospital-cardiac arrest (OHCA), JW was estimated to have been in full cardiac arrest for at least 10-15 minutes before paramedics arrived at his side. His survival and continuing health can be attributed to prompt efforts to resuscitate him, including the use of therapeutic hypothermia (TH), a procedure that reduces core body temperature while the subject is still unconscious after undergoing resuscitation from cardiac arrest. Though the physiologic basis of therapeutic hypothermia has been well-founded for a long time, its worldwide implementation for OHCA is fairly recent.
HISTORY
The need to maintain warm body temperature to sustain life is as ancient as the Old Testament. The episode involving the prophet Elisha may have derived from an instance in which a hypothermic, comatose child was rewarmed and then reawakened. There is even a hint of mouth-to-mouth resuscitation.i At the other extreme, the idea that cooling a person might slow or suspend biological processes was expressed by Hippocrates (circa 400 BC), who advocated packing wounded soldiers in snow to staunch bleeding. In more recent times, the accumulation of anecdotal experience about children who fell into icy lakes or skiers who were frozen for hours before being resuscitated has long hinted at the potential medical benefit of lowering body temperature. Animal studies in dogs in the 1950's showed that mild hypothermia helped preserve brain function after head trauma. Later in that decade, neurosurgeons introduced hypothermia for the first time to permit a bloodless field for cerebral surgery. In 1971, Sir Brian Barratt-Boyes of New Zealand reported the successful use of hypothermia combined with circulatory arrest for cardiac surgery in neonates who were deemed too small for conventional cardiopulmonary bypass.1 Not be until 2002, however, did the American Heart Association (AHA) approve and recommend therapeutic hypothermia for preservation of cerebral function after OHCA.2
PHYSIOLOGY
Though hypothermia preserves cardiac function during ischemia, its main benefit in OHCA results from a reduction in the brain’s metabolic needs, which mitigates the effects of both ischemia and subsequent reperfusion. For similar reasons, TH may be beneficial in other disorders, such as encephalopathy in newborns.3
PROCEDURE
Both invasive and non-invasive methods are currently used to lower core body temperature and achieve TH. The invasive method involves femoral vein infusion of cool saline solution. There are several non-invasive methods that rely on various cooling blankets for the torso or wraps for the extremities and head; all depend on circulating water or air that is cooled in a bedside apparatus. Other devices release mist into the nasal passages to cool the head by evaporation near the brain. Regardless of whether the procedure is internal or external, the patient must be sedated to prevent shivering.4
INVASIVE COOLING
Invasive procedures for TH can cool the body more quickly and with greater accuracy than non-invasive methods.5 Accurate cooling to the desired target temperature of around 33oC is important because cooling below 32o C can result in electrolyte imbalance, cardiac arrhythmias, greater risk of infection, and hypercoagulability. The catheter method has also been shown to be better at rewarming the patient smoothly. Most deaths during TH occur during rewarming because rewarming that is not gradual enough can result in spikes in intracranial pressure.5 Nonetheless, recent retrospective studies have also cautioned against prolonged rewarming.6
The invasive method is not without its drawbacks. Along with the typical complications of catheters such as infections and bleeding, there is a greater risk of deep vein thrombosis and pulmonary embolism due to hypercoagulability. Additionally, this procedure must be regularly overseen by a physician whereas the non-invasive methods need not be.4
NON-INVASIVE COOLING
Non-invasive cooling methods tend to be less accurate and slower, but the technology is improving and the list of potential complications is diminishing. Current cooling blankets monitor the patient’s body temperature and regulate the cooling automatically. Though rewarming is slower than with invasive methods, monitoring is not as intensive and there is no need for constant physician oversight.
PROCEDURES AT LANCASTER GENERAL HOSPITAL
Lancaster General uses external methods such as cooling blankets and leg wraps. Cooling is often begun in the cardiac catheterization lab and is typically accompanied by some form of percutaneous coronary intervention.
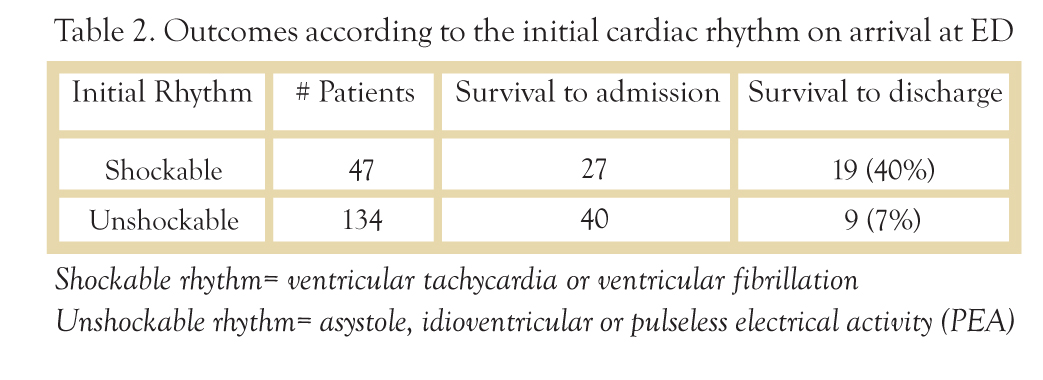
Depending on the emergency vehicle’s response time and the distance from the site of the cardiac arrest, TH can be initiated in the hospital before or after the restoration of spontaneous circulation. Candidates for the maintenance of TH must have been resuscitated following cardiac arrest, have not regained consciousness, and generally have had ventricular fibrillation associated with myocardial infarction. At least one study has shown that TH is not beneficial in patients with a non-shockable rhythm.7
EXPERIENCE AT LANCASTER GENERAL HOSPITAL
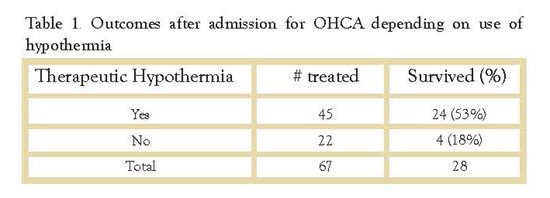
The most recent data available from LGH are from January 1, 2010 to November 30, 2012. During this period 181 patients were brought to the emergency room following an episode of OHCA. Of that number, 67 (37%) survived to be admitted, and overall, 28 of the 67 were eventually discharged. The survival rate differed markedly between the 45 who received TH and the 22 who, for whatever reason (regained consciousness, underlying illness etc.), did not.
Of the 67 patients who were admitted, 45 were treated with therapeutic hypothermia and 22 were not. 53% (24/45) of the TH patients survived to discharge with moderate to good neurologic function. In the untreated group, only 18% (4/22) survived to discharge. (Table 1) The outcome was also impacted significantly by the initial rhythm. (Table 2)
CURRENT RESEARCH
Many current studies focus on the long-term outcomes after TH. Dumas and co-workers reported 5-year survival rates in almost 6000 individuals treated with percutaneous coronary intervention and therapeutic hypothermia.8 Compared with the control group of similar patients who did not receive TH, approximately 17% more of those who arrived at the hospital and received TH following resuscitation lived for at least 5-years following their cardiac arrest.
CONCLUSION
Therapeutic hypothermia has been in use at Lancaster General Hospital for more than 5 years. The data from treated patients are still being analyzed, but early analyses suggest survival rates above 50 % in treated patients, and it already seems clear that utilization of this procedure will increase. This procedure is truly lifesaving for certain patients such as the Scoutmaster, since historically less than 30% leave the hospital alive.9
Undoubtedly, the indications and techniques for this procedure will change as experience accumulates and new research emerges. Already, researchers are looking at the efficacy of administering TH en route to the hospital. Such a protocol might save time and keep even more scoutmasters alive in the future. Along with the remainder of JW’s Eagle Scouts, this author is just glad such a procedure exists.
ACKNOWLEDGMENT
The authors thank Kim Bahata, Director of Clinical Decision Support, for providing the data from LGH.
NOTES
i 2 Kings, 4:32-36. When Elisha came into the house, he saw the child lying dead on his bed. So he went in and shut the door behind the two of them and prayed to the Lord. Then he went up and lay on the child, putting his mouth on his mouth, his eyes on his eyes, and his hands on his hands. And as he stretched himself upon him, the flesh of the child became warm. Then he got up again and walked once back and forth in the house, and went up and stretched himself upon him. The child sneezed seven times, and the child opened his eyes.
REFERENCES
1. Barratt-Boyes BG, Simpson M, Neutze JM. Intracardiac surgery in neonates and infants using deep hypothermia with surface cooling and limited cardiopulmonary bypass. Circulation. 1971;43( Suppl 5):I 25-30.
2. Polderman, KH, Application of therapeutic hypothermia in the ICU: opportunities and pitfalls of a promising treatment modality. Intensive Care Med. 2004; 30: 556-575.
3. Larson, JE and McElwee, D. Hypothermia for neuroprotection in the newborn. J Lanc Gen Hosp, 2011. 6: 74-77.
4. Hoedemaekers, CW, et al. Comparison of cooling methods to induce and maintain normo- and hypothermia in intensive care unit patients: a prospective intervention study. Critical Care, 2007. 11.
5. Calver, P, et al., The big chill: Improving the odds after cardiac arrest. Modern Medicine, 2005.
6. Benz-Woerner, J, et al. Body temperature regulation and outcome after cardiac arrest and therapeutic hypothermia. Resuscitation, 2012. 83(3): 338-342.
7. Dumas, F, et al., Is hypothermia after cardiac arrest effective in both shockable and nonshockable patients? Circulation, 2011. 123: 877-886.
8. Dumas, F., et al., Long-term prognosis following resuscitation from out of hospital cardiac arrest. J Am Coll Cardiol. 2012; 60(1): 21-27.
9. Bernard, SA, et al., Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. New Eng J Med. 2002; 346(8): 557-563.